Depression drives sugar cravings, study finds
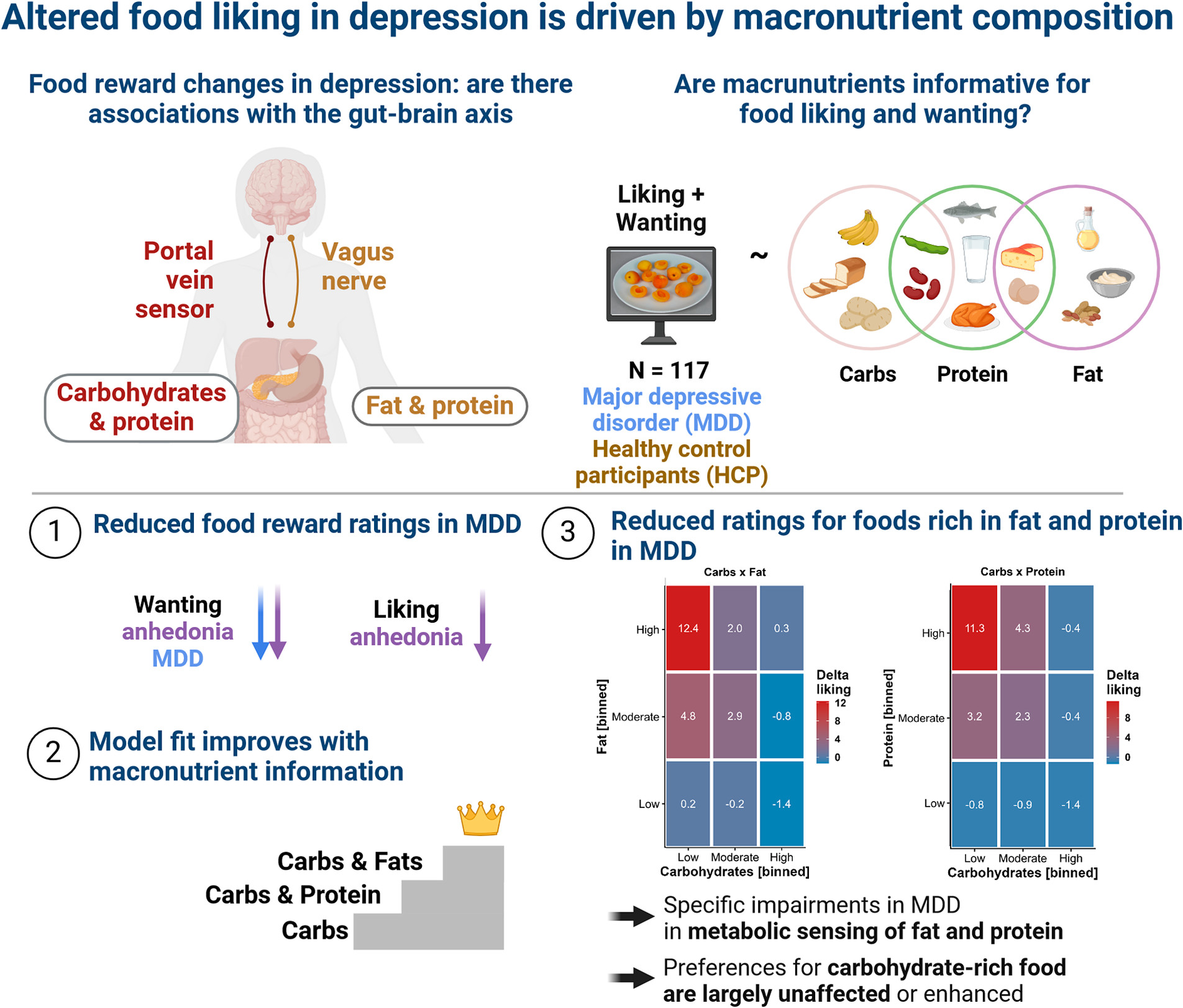
Depression doesn’t just affect mood — it changes how people eat, with new research showing that patients significantly favor carbohydrate-rich foods even when their overall appetite decreases.
The groundbreaking study, published in Psychological Medicine, challenges previous assumptions about the relationship between depression and eating habits, revealing that the craving for carbohydrates is tied more closely to the severity of depression symptoms than to increased appetite.
“Many people with depression suffer from a general loss of appetite. Others have more appetite during a depressive episode and even develop food cravings — especially for sweets,” said Professor Nils Kroemer, lead researcher at the University Hospital of Tübingen’s Department of Translational Psychiatry.
The research team found that depressed individuals showed decreased interest in protein and fat-rich foods compared to healthy control groups. However, they demonstrated a marked preference for carbohydrate-heavy options, particularly foods that combine carbohydrates and fats, such as milk chocolate.
“We were able to show that carbohydrate cravings are more related to the overall severity of depression, especially anxiety symptoms,” said Lilly Thurn, the study’s first author and former researcher at the University Hospital Bonn.
This discovery could open new avenues for treatment. Researchers are particularly interested in therapies targeting the gut-brain connection, with preliminary studies suggesting that fasting or probiotic foods might have antidepressant effects.
The findings are especially significant given that depression affects 280 million people worldwide. They suggest that dietary intervention could play a crucial role in future treatment approaches.
The research, funded by the German Research Foundation, involved collaboration between the university hospitals in Bonn and Tübingen, the German Center for Mental Health, and the Institute of Nutrition and Food Sciences at the University of Bonn.
Kroemer and his team are now exploring whether optimizing patients’ diets could lead to lasting improvements in depression symptoms. The study also revealed that depressed patients show alterations in their gut microbiome that might exacerbate various symptoms, pointing to potential new therapeutic strategies.
As mental health practitioners increasingly recognize the complex relationship between diet and depression, this research could herald a new era of integrated treatment approaches that consider both psychological and nutritional factors.



